Midwood Addiction Treatment Center, a leading rehabilitation facility in North Carolina, specializes in providing comprehensive mental health treatments and holistic approaches to drug and alcohol rehab. The center boasts state-of-the-art treatment options and a dedicated team of seasoned professionals committed to assisting patients on their path to recovery and sobriety.
The cost of addiction treatment of this type in North Carolina can vary depending on different factors, such as the duration of the treatment program and specific treatment services. On average, outpatient rehab programs may range from $1,000 to $10,000, while inpatient programs can cost anywhere from $5,000 to $30,000 or more. Our compassionate team of professionals at Midwood Addiction Treatment Center in Charlotte, North Carolina, can help patients find affordable ways to deal with their addiction treatment costs.
To find out more about alcohol and drug addiction rehab costs, you can call us at 888-399-7556 or verify your insurance coverage online. With our holistic approach to behavioral health treatment, contacting us at Midwood Drug and Alcohol Addiction Treatment Center is the first step on your path to recovery.
What Is an Addiction Treatment Center?
An addiction treatment center is a specialized treatment facility designed to address and assist individuals struggling with substance abuse or behavioral addictions. These treatment centers play an important role in providing structured and evidence-based interventions to help patients overcome their dependencies and find lasting sobriety.
The primary focus of these facilities is to offer a supportive environment where patients can undergo comprehensive treatment programs tailored to their specific needs. Typically, addiction treatment centers employ a multidisciplinary approach, incorporating medical, psychological, and social components to address the complex nature of addiction. Medical professionals, therapists, and counselors collaborate to create personalized treatment plans, which may include medication-assisted detoxification, counseling sessions, group therapy, and aftercare support. The goal of these centers is not only to address the immediate challenges of addiction but also to equip individuals with the necessary tools and coping strategies for long-term recovery.
At Midwood Addiction Treatment Center, our team plays an essential role in helping break the cycle of addiction by providing hope and facilitating the journey toward a healthier and substance-free life for our patients. To learn more about our addiction treatment programs, you can contact us online or call 888-399-7556.
How Much Does Substance Addiction Treatment Cost in North Carolina?
The cost of substance addiction treatment in North Carolina can vary widely, ranging from a few thousand to tens of thousands of dollars. Factors influencing the average cost of rehabilitation expenses include the type of treatment facility (inpatient care or outpatient care), the duration of the program, and the specific services offered.
Outpatient programs, where individuals attend therapy sessions while living at home, generally cost less than inpatient programs, which provide residential care and a more immersive treatment experience. However, it’s important to note that the average cost is a generalization, as the actual expenses can vary significantly based on the type of substance, the severity of the addiction, and the chosen treatment approach. For instance, the cost of treating addiction to alcohol may differ from that of opioids or stimulants. The severity of the addiction, whether mild, moderate, or severe, also influences the intensity and duration of treatment, impacting overall addiction treatment affordability.
Additionally, the choice between standard outpatient care, intensive outpatient programs, or residential inpatient treatment further contributes to the variability in addiction recovery costs. As such, individuals considering addiction treatment in North Carolina should carefully assess their unique needs and treatment program fees to determine the most suitable and cost-effective option for their recovery journey. At Midwood Substance Addiction Treatment Center, we can help you verify your insurance coverage, determine your therapy program expenses, and examine the overall cost of addiction therapy for you.

Midwood Addiction Treatment Center
Contact us to schedule a free assessment.
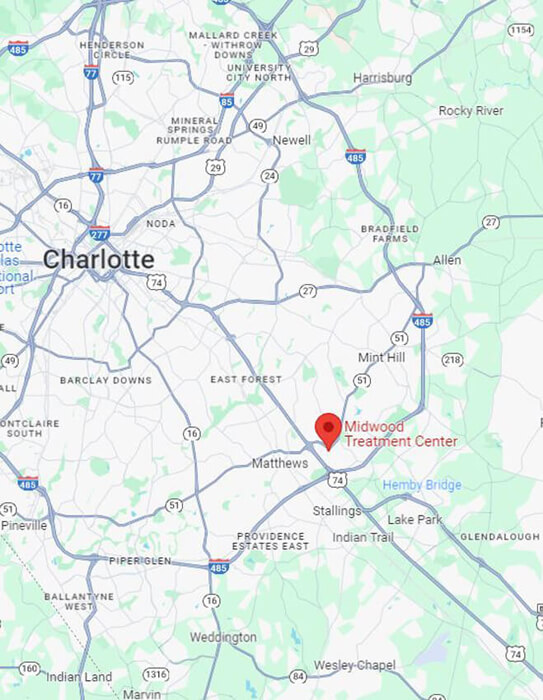
Located just minutes from the heart of Charlotte, our treatment center is a warm, welcoming place supporting recovery. The facility includes various group rooms, therapist and case management offices, and medical offices, among other amenities. All clinical and medical services, from intake and assessment to discharge, are provided within our treatment center.
Substance Abuse Center in North Carolina That Offers Payment Plans
Midwood Addiction Treatment Center in North Carolina is a substance abuse treatment facility that recognizes the financial challenges individuals may face when seeking help for addiction. Understanding the importance of accessibility to quality care, Midwood Addiction Center stands out by accepting insurance plans and helping make addiction treatment more affordable and attainable for those in need.
In addition to accepting many different types of insurance plans, Midwood Alcohol and Drug Addiction Treatment Center further enhances affordability by offering flexible payment plans. These payment options allow individuals to manage the financial aspects of their treatment over time, making it more feasible for those who may not have the means to cover the entire cost upfront. By providing both insurance acceptance and payment plans, Midwood Addiction Center strives to break down financial barriers, ensuring that individuals have access to the comprehensive and supportive care they need to overcome substance abuse challenges and embark on a path to recovery.
Midwood Addiction Treatment Center
3057 Senna Drive
Matthews, NC 28105
Phone: 888-399-7556
Website: Midwood Drug and Alcohol Addiction Treatment Center
Cost of Alcohol Use Disorder Treatment in NC
The cost of Alcohol Use Disorder (AUD) treatment depends on several factors, including the type of treatment facility, the duration of the program, and the specific services provided. On average, outpatient programs in North Carolina may range from several hundred to several thousand dollars, offering flexibility for individuals to attend therapy sessions while residing at home.
Meanwhile, residential inpatient rehab programs, which provide a more immersive and structured treatment experience, typically incur higher costs, ranging from several thousand to tens of thousands of dollars. Understanding the cost of AUD treatment in North Carolina is crucial for individuals seeking help.
The actual cost of alcohol use disorder (AUD) treatment can depend on individual circumstances. Factors such as the severity of alcohol use, the chosen treatment approach, and whether insurance coverage is available can all influence the overall expenses. Many treatment centers in North Carolina accept insurance, potentially mitigating some of the financial burden for individuals seeking help for alcohol-related challenges.
At Midwood Addiction Treatment Center, in addition to accepting a range of insurance plans, we also offer payment plans to help make drug and alcohol rehab costs more affordable for our patients and ensure that cost is not a barrier to accessing crucial treatment services.
Cost of Opioid Use Disorder Treatment in NC
The cost of opioid use disorder (OUD) treatment in North Carolina can vary based on several factors, including the type of treatment facility, the intensity and duration of the program, and the specific services rendered. On average, outpatient programs in North Carolina may range from a few thousand to several thousand dollars, providing individuals with the flexibility to attend therapy sessions while residing at home.
In contrast, inpatient rehab programs for opioid use disorder, which offer a more immersive and structured treatment environment, generally incur higher costs, ranging from several thousand to tens of thousands of dollars. The actual substance use disorder treatment costs can also be influenced by individual factors such as the severity of the addiction, the chosen treatment modalities, and the availability of insurance coverage.
Midwood Addiction Treatment Center in North Carolina offers many different rehabilitation financing options. In addition to accepting a wide range of insurance plans, we also offer addiction treatment payment plans or sliding scale fees to help make drug and alcohol rehab costs more affordable for our patients and ensure that cost is not a barrier to accessing crucial treatment services.
Cost of Cocaine Use Disorder Treatment in NC
The cost of cocaine use disorder (CUD) treatment in North Carolina can vary based on factors such as the type of treatment facility, the duration and intensity of the program, and the specific services provided. Typically, outpatient programs in North Carolina can cost anywhere from a few thousand to several thousand dollars.
On the other hand, inpatient programs, known for their more comprehensive and structured treatment approach, tend to incur higher expenses, ranging from several thousand to tens of thousands of dollars. Individual circumstances also play a significant role in determining the actual cost of cocaine use disorder (CUD) treatment. The severity of the cocaine use disorder, the chosen treatment modalities, and the availability of insurance coverage all contribute to the overall expenses.
Midwood Drug and Alcohol Addiction Treatment Center provides diverse financing options for rehabilitation. Beyond accepting various health insurance plans, we extend addiction treatment payment plans and sliding scale fees. This approach aims to enhance affordability for our patients, ensuring that the costs associated with drug and alcohol rehab do not pose a barrier to accessing essential treatment services. For more information, you can contact us online or call 888-399-7556.
Cost of Heroin Addiction Treatment in NC
The expenses associated with heroin addiction Treatment in North Carolina can fluctuate based on factors like the type of treatment facility, program duration, and intensity, as well as the specific services offered. The cost of outpatient rehab programs in North Carolina may range from a few thousand to several thousand dollars, while inpatient programs cost more.
Inpatient rehab programs, known for their more comprehensive and structured treatment, usually involve higher costs, ranging from several thousand to tens of thousands of dollars. The actual cost of heroin addiction treatment is also influenced by individual factors such as the severity of the addiction, chosen treatment methods, and insurance coverage.
Midwood Substance Addiction Treatment Center offers various financing options for heroin addiction treatment and rehabilitation. Apart from accepting different health insurance plans, we provide payment plans and sliding scale fees for heroin treatment to enhance affordability for our patients, ensuring that the financial aspect does not hinder access to essential treatment services. For further details, you can contact us online or call us.
Cost of Methamphetamine Use Disorder Treatment in NC
The cost of methamphetamine use disorder treatment can vary depending on factors such as the type of treatment facility, program duration, and the specific services offered. Typically, outpatient programs in North Carolina may range from several hundred to several thousand dollars, while residential inpatient rehab programs generally incur higher costs, ranging from several thousand to tens of thousands of dollars.
The actual cost of methamphetamine use disorder treatment depends on individual circumstances. Factors like the severity of the disorder, chosen treatment methods, and insurance coverage availability can significantly impact overall expenses. Many treatment centers in North Carolina accept insurance, potentially easing some of the financial burden for individuals seeking help for methamphetamine-related challenges.
At Midwood Addiction Treatment Center, aside from accepting various health insurance plans, we provide payment plans or sliding scale fees so we can offer more affordable addiction treatment for our patients dealing with methamphetamine use disorder. To learn more about our treatment options for methamphetamine addiction, you can contact us online or call us.
Cost of Cannabis Use Disorder Treatment in NC
The cost of cannabis use disorder (CUD) treatment in North Carolina can vary based on several factors, including the type of treatment facility, the duration and intensity of the treatment and recovery program, and the specific marijuana addiction treatment services provided.
Generally, marijuana rehab outpatient programs in North Carolina range in cost from a few hundred to several thousand dollars, allowing individuals the flexibility to attend therapy sessions while residing at home. In contrast, inpatient rehab programs, known for their more immersive and structured treatment approach, may have higher addiction treatment costs, ranging from several thousand to tens of thousands of dollars.
Recognizing the evolving landscape around cannabis, Midwood Addiction Treatment Center in Charlotte, North Carolina, offers affordable substance abuse treatment pricing for marijuana use treatment services so that patients can keep their overall rehabilitation expenses down. If you or someone you know needs help dealing with marijuana addiction treatment or cannabis use disorder (CUD) treatment in North Carolina, you can call the Midwood Addiction Treatment Center in Charlotte or contact us online.
Cost of Benzodiazepine Use Disorder Treatment in NC
The expenses associated with benzodiazepine use disorder (BUD) treatment in North Carolina can vary, contingent on factors like the treatment facility type, the duration and intensity of the treatment and recovery program, and the specific services provided to address benzodiazepine addiction.
Generally, outpatient programs designed for benzodiazepine rehab in North Carolina may range from a few hundred to several thousand dollars, while inpatient rehab programs, known for their immersive and structured treatment approach, usually incur higher costs for managing benzodiazepine addiction, ranging from several thousand to tens of thousands of dollars.
Acknowledging the distinctive challenges associated with benzodiazepine use, Midwood Substance Addiction Treatment Center provides cost-effective substance abuse treatment pricing options for benzodiazepine use disorder treatment services, ensuring that patients can effectively manage their rehabilitation expenses. If you or someone you know needs assistance with benzodiazepine addiction treatment in North Carolina, contact us at Midwood Addiction Treatment Center or call 888-399-7556.
Should I Pay for Addiction Treatment If I Don’t Have Insurance?
Paying for addiction treatment, even without insurance, can be a wise investment with substantial long-term benefits. The health benefits of undergoing professional addiction treatment are paramount. Addressing addiction in a structured and supportive environment increases the likelihood of successful recovery, significantly improving physical and mental well-being.
Investing in treatment enhances the prospects of breaking free from the cycle of addiction, leading to a healthier and more fulfilling life. Moreover, the long-term financial benefits of addiction treatment are substantial. While the initial cost of addiction treatment may seem significant, the expenses associated with untreated addiction, such as medical complications, legal issues, and lost productivity, can far exceed the investment in professional treatment. By addressing addiction early on, individuals can prevent the compounding financial burdens that often accompany untreated substance abuse.
Choosing to pay for addiction treatment is an investment not only in one’s health but also in long-term financial stability and overall well-being. If you are considering addiction treatment without insurance, contact us at Midwood Addiction Treatment Center to explore rehab expense breakdown and discuss how investing in your recovery can lead to a brighter future.

Does Insurance Pay For Addiction Treatment in North Carolina?
Yes, insurance typically covers addiction treatment in North Carolina. Many health insurance plans provide coverage for various aspects of addiction treatment, including medical detoxification, outpatient and inpatient rehabilitation, counseling, and aftercare services. However, the extent of coverage can vary depending on the insurance plan, so it’s crucial to review the policy details for clarity on what is covered.
If you seek addiction treatment in North Carolina, you can verify your insurance coverage online through Midwood Addiction Treatment Center. If you have additional questions about insurance coverage for addiction treatment or out-of-pocket rehab expenses or need assistance understanding your options, please contact us online or call 888-399-7556. Our dedicated team is here to provide guidance and support throughout the rehab process.
How To Pay For Drug or Alcohol Addiction Treatment Without Insurance
Paying for drug or alcohol addiction treatment without insurance can be challenging, but there are viable options to make it accessible. Many reputable treatment centers, including Midwood Drug and Alcohol Addiction Treatment Center, offer various payment plans and financial assistance programs to accommodate individuals seeking help.
These options aim to alleviate the financial burden, ensuring that cost doesn’t hinder someone from getting the necessary care for their recovery journey. If you or a loved one is considering addiction treatment without insurance coverage, don’t hesitate to reach out to us at Midwood Addiction Treatment Center. Our compassionate and experienced team is available to discuss rehab financial planning options and guide you through the process. Call us today at 888-399-7556 or contact us online, and let’s explore how we can help you or your loved one embark on the path to recovery without the constraints of insurance limitations.
Financial Consequences of Addiction Issues
What Is the Cost of Alcohol Addiction in North Carolina?
What Is the Cost of Drug Addiction in North Carolina?
Contact Midwood Addiction Treatment Center
Consult our compassionate experts to help you find a roadmap to addiction recovery.